Addison’s Disease and Adrenal Insufficiency
What is adrenal insufficiency?
Adrenal insufficiency is an endocrine, or hormonal, disorder that occurs when the adrenal glands do not produce enough of certain hormones. The adrenal glands are located just above the kidneys.
Adrenal insufficiency can be primary or secondary. Addison’s disease, the common term for primary adrenal insufficiency, occurs when the adrenal glands are damaged and cannot produce enough of the adrenal hormone cortisol. The adrenal hormone aldosterone may also be lacking. Addison’s disease affects 110 to 144 of every 1 million people in developed countries.
Secondary adrenal insufficiency occurs when the pituitary gland—a pea-sized gland at the base of the brain—fails to produce enough adrenocorticotropin (ACTH), a hormone that stimulates the adrenal glands to produce the hormone cortisol. If ACTH output is too low, cortisol production drops. Eventually, the adrenal glands can shrink due to lack of ACTH stimulation. Secondary adrenal insufficiency is much more common than Addison’s disease.
What do adrenal hormones do?
Adrenal hormones, such as cortisol and aldosterone, play key roles in the functioning of the human body, such as regulating blood pressure; metabolism, the way the body uses digested food for energy; and the body’s response to stress. In addition, the body uses the adrenal hormone dehydroepiandrosterone (DHEA) to make androgens and estrogens, the male and female sex hormones.
Cortisol
Cortisol belongs to the class of hormones called glucocorticoids, which affect almost every organ and tissue in the body. Cortisol’s most important job is to help the body respond to stress. Among its many tasks, cortisol helps
- maintain blood pressure and heart and blood vessel function
- slow the immune system’s inflammatory response—how the body recognizes and defends itself against bacteria, viruses, and substances that appear foreign and harmful
- regulate metabolism
The amount of cortisol produced by the adrenal glands is precisely balanced.
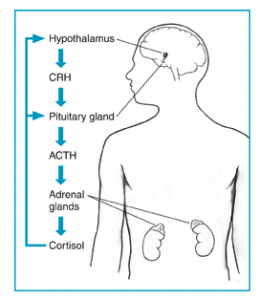
Like many other hormones, cortisol is regulated by the hypothalamus, which is a part of the brain, and the pituitary gland. First, the hypothalamus releases a “trigger” hormone called corticotropin-releasing hormone (CRH), which signals the pituitary gland to send out ACTH. ACTH stimulates the adrenal glands to produce cortisol. Cortisol then signals back to both the pituitary gland and hypothalamus to decrease these trigger hormones. The amount of cortisol produced by the adrenal glands is precisely balanced.
Aldosterone
Aldosterone belongs to the class of hormones called mineralocorticoids, also produced by the adrenal glands. Aldosterone helps maintain blood pressure and the balance of sodium and potassium in the blood. When aldosterone production falls too low, the body loses too much sodium and retains too much potassium.
The decrease of sodium in the blood can lead to a drop in both blood volume—the amount of fluid in the blood—and blood pressure. Too little sodium in the body also can cause a condition called hyponatremia. Symptoms of hyponatremia include feeling confused and fatigued and having muscle twitches and seizures.
Too much potassium in the body can lead to a condition called hyperkalemia. Hyperkalemia may have no symptoms; however, it can cause irregular heartbeat, nausea, and a slow, weak, or an irregular pulse.
Dehydroepiandrosterone
Dehydroepiandrosterone is another hormone produced by the body’s adrenal glands. The body uses DHEA to make the sex hormones, androgen and estrogen. With adrenal insufficiency, the adrenal glands may not make enough DHEA. Healthy men derive most androgens from the testes. Healthy women and adolescent girls get most of their estrogens from the ovaries. However, women and adolescent girls may have various symptoms from DHEA insufficiency, such as loss of pubic hair, dry skin, a reduced interest in sex, and depression.
What are the symptoms of adrenal insufficiency and adrenal crisis?
Adrenal Insufficiency
The most common symptoms of adrenal insufficiency are:
- chronic, or long lasting, fatigue
- muscle weakness
- loss of appetite
- weight loss
- abdominal pain
Other symptoms of adrenal insufficiency can include:
- nausea
- vomiting
- diarrhea
- low blood pressure that drops further when a person stands up, causing dizziness or fainting
- irritability and depression
- craving salty foods
- hypoglycemia, or low blood sugar
- headache
- sweating
- irregular or absent menstrual periods
- in women, loss of interest in sex
Hyperpigmentation, or darkening of the skin, can occur in Addison’s disease, although not in secondary adrenal insufficiency. This darkening is most visible on scars; skin folds; pressure points such as the elbows, knees, knuckles, and toes; lips; and mucous membranes such as the lining of the cheek.
The slowly progressing symptoms of adrenal insufficiency are often ignored until a stressful event, such as surgery, a severe injury, an illness, or pregnancy, causes them to worsen.
Adrenal Crisis
Sudden, severe worsening of adrenal insufficiency symptoms is called adrenal crisis. If the person has Addison’s disease, this worsening can also be called an Addisonian crisis. In most cases, symptoms of adrenal insufficiency become serious enough that people seek medical treatment before an adrenal crisis occurs. However, sometimes symptoms appear for the first time during an adrenal crisis.
Symptoms of adrenal crisis include
- sudden, severe pain in the lower back, abdomen, or legs
- severe vomiting and diarrhea
- dehydration
- low blood pressure
- loss of consciousness
If not treated, an adrenal crisis can cause death.
Get Treatment for Adrenal Crisis Right Away
People with adrenal insufficiency who have weakness, nausea, or vomiting need immediate emergency treatment to prevent an adrenal crisis and possible death. An injection with a synthetic glucocorticoid hormone called a corticosteroid can save a person’s life. People should make sure to have a corticosteroid injection with them at all times, and make sure their friends and family know how and when to give the injection.
Read more under “How is adrenal insufficiency treated?”
What causes Addison’s disease?
Autoimmune disorders cause most cases of Addison’s disease. Infections and medications may also cause the disease.
Autoimmune Disorders
Up to 80 percent of Addison’s disease cases are caused by an autoimmune disorder, which is when the body’s immune system attacks the body’s own cells and organs. In autoimmune Addison’s, which mainly occurs in middle-aged females, the immune system gradually destroys the adrenal cortex—the outer layer of the adrenal glands.
Primary adrenal insufficiency occurs when at least 90 percent of the adrenal cortex has been destroyed. As a result, both cortisol and aldosterone are often lacking. Sometimes only the adrenal glands are affected. Sometimes other endocrine glands are affected as well, as in polyendocrine deficiency syndrome.
Polyendocrine deficiency syndrome is classified into type 1 and type 2.
Type 1 is inherited and occurs in children. In addition to adrenal insufficiency, these children may have
- underactive parathyroid glands, which are four pea-sized glands located on or near the thyroid gland in the neck; they produce a hormone that helps maintain the correct balance of calcium in the body.
- slow sexual development.
- pernicious anemia, a severe type of anemia; anemia is a condition in which red blood cells are fewer than normal, which means less oxygen is carried to the body’s cells. With most types of anemia, red blood cells are smaller than normal; however, in pernicious anemia, the cells are bigger than normal.
- chronic fungal infections.
- chronic hepatitis, a liver disease.
Researchers think type 2, which is sometimes called Schmidt’s syndrome, is also inherited. Type 2 usually affects young adults and may include
- an underactive thyroid gland, which produces hormones that regulate metabolism
- slow sexual development
- diabetes, in which a person has high blood glucose, also called high blood sugar or hyperglycemia
- vitiligo, a loss of pigment on areas of the skin
Infections
Tuberculosis (TB), an infection that can destroy the adrenal glands, accounts for 10 to 15 percent of Addison’s disease cases in developed countries.1 When primary adrenal insufficiency was first identified by Dr. Thomas Addison in 1849, TB was the most common cause of the disease. As TB treatment improved, the incidence of Addison’s disease due to TB of the adrenal glands greatly decreased. However, recent reports show an increase in Addison’s disease from infections such as TB and cytomegalovirus. Cytomegalovirus is a common virus that does not cause symptoms in healthy people; however, it does affect babies in the womb and people who have a weakened immune system—mostly due to HIV/AIDS.2 Other bacterial infections, such as Neisseria meningitidis, which is a cause of meningitis, and fungal infections can also lead to Addison’s disease.
Other Causes
Less common causes of Addison’s disease are
- cancer cells in the adrenal glands
- amyloidosis, a serious, though rare, group of diseases that occurs when abnormal proteins, called amyloids, build up in the blood and are deposited in tissues and organs
- surgical removal of the adrenal glands
- bleeding into the adrenal glands
- genetic defects including abnormal adrenal gland development, an inability of the adrenal glands to respond to ACTH, or a defect in adrenal hormone production
- medication-related causes, such as from anti-fungal medications and the anesthetic etomidate, which may be used when a person undergoes an emergency intubation—the placement of a flexible, plastic tube through the mouth and into the trachea, or windpipe, to assist with breathing
What causes secondary adrenal insufficiency?
A lack of CRH or ACTH causes secondary adrenal insufficiency. The lack of these hormones in the body can be traced to several possible sources.
Stoppage of Corticosteroid Medication
A temporary form of secondary adrenal insufficiency may occur when a person who has been taking a synthetic glucocorticoid hormone, called a corticosteroid, for a long time stops taking the medication. Corticosteroids are often prescribed to treat inflammatory illnesses such as rheumatoid arthritis, asthma, and ulcerative colitis. In this case, the prescription doses often cause higher levels than those normally achieved by the glucocorticoid hormones created by the body. When a person takes corticosteroids for prolonged periods, the adrenal glands produce less of their natural hormones. Once the prescription doses of corticosteroid are stopped, the adrenal glands may be slow to restart their production of the body’s glucocorticoids. To give the adrenal glands time to regain function and prevent adrenal insufficiency, prescription corticosteroid doses should be reduced gradually over a period of weeks or even months. Even with gradual reduction, the adrenal glands might not begin to function normally for some time, so a person who has recently stopped taking prescription corticosteroids should be watched carefully for symptoms of secondary adrenal insufficiency.
Surgical Removal of Pituitary Tumors
Another cause of secondary adrenal insufficiency is surgical removal of the usually noncancerous, ACTH-producing tumors of the pituitary gland that cause Cushing’s syndrome. Cushing’s syndrome is a hormonal disorder caused by prolonged exposure of the body’s tissues to high levels of the hormone cortisol. When the tumors are removed, the source of extra ACTH is suddenly gone and a replacement hormone must be taken until the body’s adrenal glands are able to resume their normal production of cortisol. The adrenal glands might not begin to function normally for some time, so a person who has had an ACTH-producing tumor removed and is going off of his or her prescription corticosteroid replacement hormone should be watched carefully for symptoms of adrenal insufficiency.
Read more in Cushing’s Syndrome at www.endocrine.niddk.nih.gov
Changes in the Pituitary Gland
Less commonly, secondary adrenal insufficiency occurs when the pituitary gland either decreases in size or stops producing ACTH. These events can result from
- tumors or an infection in the pituitary
- loss of blood flow to the pituitary
- radiation for the treatment of pituitary or nearby tumors
- surgical removal of parts of the hypothalamus
- surgical removal of the pituitary
How is adrenal insufficiency diagnosed?
In its early stages, adrenal insufficiency can be difficult to diagnose. A health care provider may suspect it after reviewing a person’s medical history and symptoms.
A diagnosis of adrenal insufficiency is confirmed through hormonal blood and urine tests. A health care provider uses these tests first to determine whether cortisol levels are too low and then to establish the cause. Imaging studies of the adrenal and pituitary glands can be useful in helping to establish the cause.
A lab technician performs the following tests in a health care provider’s office, a commercial facility, or a hospital.
Hormonal Blood and Urine Tests
- ACTH stimulation test. The ACTH stimulation test is the most commonly used test for diagnosing adrenal insufficiency. In this test, the patient is given an intravenous (IV) injection of synthetic ACTH, and samples of blood, urine, or both are taken before and after the injection. The cortisol levels in the blood and urine samples are measured in a lab. The normal response after an ACTH injection is a rise in blood and urine cortisol levels. People with Addison’s disease or longstanding secondary adrenal insufficiency have little or no increase in cortisol levels.Both low- and high-dose ACTH stimulation tests may be used depending on the suspected cause of adrenal insufficiency. For example, if secondary adrenal insufficiency is mild or has only recently occurred, the adrenal glands may still respond to ACTH because they have not yet shut down their own production of hormone. Some studies have suggested a low dose—1 microgram (mcg)—may be more effective in detecting secondary adrenal insufficiency because the low dose is still enough to raise cortisol levels in healthy people, yet not in people with mild or recent secondary adrenal insufficiency. However, recent research has shown that a significant proportion of healthy children and adults can fail the low-dose test, which may lead to unnecessary treatment. Therefore, some health care providers favor using a 250 mcg ACTH test for more accurate results.
- CRH stimulation test. When the response to the ACTH test is abnormal, a CRH stimulation test can help determine the cause of adrenal insufficiency. In this test, the patient is given an IV injection of synthetic CRH, and blood is taken before and 30, 60, 90, and 120 minutes after the injection. The cortisol levels in the blood samples are measured in a lab. People with Addison’s disease respond by producing high levels of ACTH, yet no cortisol. People with secondary adrenal insufficiency do not produce ACTH or have a delayed response. CRH will not stimulate ACTH secretion if the pituitary is damaged, so no ACTH response points to the pituitary as the cause. A delayed ACTH response points to the hypothalamus as the cause.
Diagnosis during Adrenal Crisis
Although a reliable diagnosis is not possible during adrenal crisis, measurement of blood ACTH and cortisol during the crisis—before treatment with corticosteroids is given—is often enough to make a preliminary diagnosis. Low blood sodium, low blood glucose, and high blood potassium are also sometimes present at the time of adrenal crisis. Once the crisis is controlled, an ACTH stimulation test can be performed to help make a specific diagnosis. More complex lab tests are sometimes used if the diagnosis remains unclear.
What other tests might a health care provider perform after diagnosis of adrenal insufficiency?
After Addison’s disease is diagnosed, health care providers may use the following tests to look at the adrenal glands, find out whether the disease is related to TB, or identify antibodies associated with autoimmune Addison’s disease.
- Ultrasound of the abdomen. Ultrasound uses a device, called a transducer, that bounces safe, painless sound waves off organs to create an image of their structure. A specially trained technician performs the procedure in a health care provider’s office, an outpatient center, or a hospital, and a radiologist—a doctor who specializes in medical imaging—interprets the images; a patient does not need anesthesia. The images can show abnormalities in the adrenal glands, such as enlargement or small size, nodules, or signs of calcium deposits, which may indicate bleeding.
- Tuberculin skin test. A tuberculin skin test measures how a patient’s immune system reacts to the bacteria that cause TB. A small needle is used to put some testing material, called tuberculin, under the skin. A nurse or lab technician performs the test in a health care provider’s office; a patient does not need anesthesia. In 2 to 3 days, the patient returns to the health care provider, who will check to see if the patient had a reaction to the test. The test can show if adrenal insufficiency could be related to TB.To test whether a person has TB infection, which is when TB bacteria live in the body without making the person sick, a special TB blood test is used. To test whether a person has TB disease, which is when TB bacteria are actively attacking a person’s lungs and making the person sick, other tests such as a chest x ray and a sample of sputum—phlegm that is coughed up from deep in the lungs—may be needed.
- Antibody blood tests. A blood test involves drawing blood at a health care provider’s office or a commercial facility and sending the sample to a lab for analysis. The blood test can detect antibodies—proteins made by the immune system to protect the body from foreign substances—associated with autoimmune Addison’s disease.
After secondary adrenal insufficiency is diagnosed, health care providers may use the following tests to obtain a detailed view of the pituitary gland and assess how it is functioning:
- Computerized tomography (CT) scan. CT scans use a combination of x rays and computer technology to create images. For a CT scan, the patient may be given a solution to drink and an injection of a special dye, called contrast medium. CT scans require the patient to lie on a table that slides into a tunnel-shaped device where the x rays are taken. An x-ray technician performs the procedure in an outpatient center or a hospital, and a radiologist interprets the images. The patient does not need anesthesia. A CT scan can show size and shape of the pituitary gland to find out if an abnormality is present.
- Magnetic resonance imaging (MRI). MRI machines use radio waves and magnets to produce detailed pictures of the body’s internal organs and soft tissues without using x rays. An MRI may include the injection of contrast medium. With most MRI machines, the patient lies on a table that slides into a tunnel-shaped device that may be open ended or closed at one end; some machines are designed to allow the patient to lie in a more open space. A specially trained technician performs the procedure in an outpatient center or a hospital, and a radiologist interprets the images. The patient does not need anesthesia, though people with a fear of confined spaces may receive light sedation, taken by mouth. MRIs can be used to produce a three-dimensional (3-D) image of the hypothalamus and the pituitary gland to find out if an abnormality is present.
- Hormonal blood tests. Hormonal blood tests can assess how the pituitary gland is functioning and its ability to produce other hormones.
How is adrenal insufficiency treated?
Adrenal insufficiency is treated by replacing, or substituting, the hormones that the adrenal glands are not making. The dose of each medication is adjusted to meet the needs of the patient.
Cortisol is replaced with a corticosteroid, such as hydrocortisone, prednisone, or dexamethasone, taken orally one to three times each day, depending on which medication is chosen.
If aldosterone is also deficient, it is replaced with oral doses of a mineralocorticoid hormone, called fludrocortisone acetate (Florinef), taken once or twice daily. People with secondary adrenal insufficiency normally maintain aldosterone production, so they do not require aldosterone replacement therapy.
During adrenal crisis, low blood pressure, low blood glucose, low blood sodium, and high blood levels of potassium can be life threatening. Standard therapy involves immediate IV injections of corticosteroids and large volumes of IV saline solution with dextrose, a type of sugar. This treatment usually brings rapid improvement. When the patient can take liquids and medications by mouth, the amount of corticosteroids is decreased until a dose that maintains normal hormone levels is reached. If aldosterone is deficient, the person will need to regularly take oral doses of fludrocortisone acetate.
Researchers have found that using replacement therapy for DHEA in adolescent girls who have secondary adrenal insufficiency and low levels of DHEA can improve pubic hair development and psychological stress. Further studies are needed before routine supplementation recommendations can be made.
What problems can occur with adrenal insufficiency?
Problems can occur in people with adrenal insufficiency who are undergoing surgery, suffer a severe injury, have an illness, or are pregnant. These conditions place additional stress on the body, and people with adrenal insufficiency may need additional treatment to respond and recover.
Surgery
People with adrenal insufficiency who need any type of surgery requiring general anesthesia must be treated with IV corticosteroids and saline. IV treatment begins before surgery and continues until the patient is fully awake after surgery and is able to take medication by mouth. The “stress” dosage is adjusted as the patient recovers until the regular, presurgery dose is reached.
In addition, people who are not currently taking corticosteroids, yet have taken long-term corticosteroids in the past year, should tell their health care provider before surgery. These people may have sufficient ACTH for normal events; however, they may need IV treatment for the stress of surgery.
Severe Injury
Patients who suffer severe injury may need a higher, “stress” dosage of corticosteroids immediately following the injury and during recovery. Often, these stress doses must be given intravenously. Once the patient recovers from the injury, dosing is returned to regular, pre-injury levels.
Illness
During an illness, a person taking corticosteroids orally may take an adjusted dose to mimic the normal response of the adrenal glands to this stress on the body. Significant fever or injury may require a triple dose. Once the person recovers from the illness, dosing is then returned to regular, pre-illness levels. People with adrenal insufficiency should know how to increase medication during such periods of stress, as advised by their health care provider. Immediate medical attention is needed if severe infections, vomiting, or diarrhea occur. These conditions can lead to an adrenal crisis.
Pregnancy
Women with adrenal insufficiency who become pregnant are treated with the same hormone therapy taken prior to pregnancy. However, if nausea and vomiting in early pregnancy interfere with taking medication orally, injections of corticosteroids may be necessary. During delivery, treatment is similar to that of people needing surgery. Following delivery, the dose is gradually lessened, and the regular dose is reached about 10 days after childbirth.
How is adrenal crisis treated?
Adrenal crisis is treated with adrenal hormones. People with adrenal crisis need immediate treatment. Any delay can cause death. When people with adrenal crisis are vomiting or unconscious and cannot take their medication, the hormones can be given as an injection.
A person with adrenal insufficiency should carry a corticosteroid injection at all times and make sure that others know how and when to administer the injection, in case the person becomes unconscious.
The dose of corticosteroid needed may vary with a person’s age or size. For example, a child younger than 2 years of age can receive 25 milligrams (mg), a child between 2 and 8 years of age can receive 50 mg, and a child older than 8 years should receive the adult dose of 100 mg.
How can a person prevent adrenal crisis?
The following steps can help a person prevent adrenal crisis:
- Ask a health care provider about possibly having a shortage of adrenal hormones, if always feeling tired, weak, or losing weight.
- Learn how to increase the dose of corticosteroid for adrenal insufficiency when ill. Ask a health care provider for written instructions for sick days. First discuss the decision to increase the dose with the health care provider when ill.
- When very ill, especially if vomiting and not able to take pills, seek emergency medical care immediately.
How can someone with adrenal insufficiency prepare in case of an emergency?
People with adrenal insufficiency should always carry identification stating their condition, “adrenal insufficiency,” in case of an emergency. A card or medical alert tag should notify emergency health care providers of the need to inject corticosteroids if the person is found severely injured or unable to answer questions.
The card or tag should also include the name and telephone number of the person’s health care provider and the name and telephone number of a friend or family member to be notified. People with adrenal insufficiency should always carry a needle, a syringe, and an injectable form of corticosteroids for emergencies.
Eating, Diet, and Nutrition
Some people with Addison’s disease who are aldosterone deficient can benefit from following a diet rich in sodium. A health care provider or a dietitian can give specific recommendations on appropriate sodium sources and daily sodium guidelines if necessary.
Corticosteroid treatment is linked to an increased risk of osteoporosis—a condition in which the bones become less dense and more likely to fracture. People who take corticosteroids should protect their bone health by consuming enough dietary calcium and vitamin D. A health care provider or a dietitian can give specific recommendations on appropriate daily calcium intake based upon age and suggest the best types of calcium supplements, if necessary.
Points to Remember
- Adrenal insufficiency is an endocrine, or hormonal, disorder that occurs when the adrenal glands do not produce enough of certain hormones.
- Addison’s disease, the common term for primary adrenal insufficiency, occurs when the adrenal glands are damaged and cannot produce enough of the adrenal hormone cortisol. The adrenal hormone aldosterone may also be lacking.
- Secondary adrenal insufficiency occurs when the pituitary gland fails to produce enough adrenocorticotropin (ACTH), a hormone that stimulates the adrenal glands to produce cortisol. If ACTH output is too low, cortisol production drops.
- The most common symptoms of adrenal insufficiency are chronic fatigue, muscle weakness, loss of appetite, weight loss, and abdominal pain. The slowly progressing symptoms are often ignored until a stressful event, such as surgery, a severe injury, an illness, or pregnancy, causes them to worsen.
- If not treated, an adrenal crisis can cause death.
- A diagnosis of adrenal insufficiency is confirmed through hormonal blood and urine tests. Imaging studies of the adrenal and pituitary glands can be useful in helping to establish the cause.
- Adrenal insufficiency is treated by replacing, or substituting, the hormones that the adrenal glands are not making.
- Problems can occur in people with adrenal insufficiency who are undergoing surgery, suffer a severe injury, have an illness, or are pregnant. These conditions place additional stress on the body, and people with adrenal insufficiency may need additional treatment to respond and recover.
- People with adrenal insufficiency should always carry identification stating their condition, “adrenal insufficiency,” in case of an emergency, as well as the supplies necessary to administer an emergency corticosteroid injection.
Hope through Research
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) conducts research on adrenal insufficiency. Scientists, funded under National Institutes of Health (NIH) clinical trial number NCT00156767, are studying the occurrence of “relative” adrenal insufficiency— below‑normal production of adrenal hormones during critical illness—to further define this type of adrenal insufficiency, develop diagnostic tests, and identify the best treatment options.
Clinical trials are research studies involving people. Clinical trials look at safe and effective new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. To learn more about clinical trials, why they matter, and how to participate, visit the NIH Clinical Research Trials and You website at www.nih.gov/health/clinicaltrialsExternal NIH Link. For information about current studies, visit www.ClinicalTrials.gov
For More Information
American Autoimmune Related Diseases Association, Inc.
22100 Gratiot Avenue
Eastpointe, MI 48021
Phone: 1–800–598–4668 or 586–776–3900
Fax: 586–776–3903
Internet: www.aarda.org
Hormone Health Network
Phone: 1–800–HORMONE (1–800–467–6663)
Email: [email protected]
Internet: www.hormone.org
National Adrenal Diseases Foundation
505 Northern Boulevard
Great Neck, NY 11021
Phone: 516–487–4992
Email: [email protected]
Internet: www.nadf.us
Addison’s Support Advocacy and Forum www.addisonssupport.com